Pericarditis
Pericarditis (PER-i-kar-DI-tis) is a condition in which the membrane, or sac, around your heart is inflamed. This sac is called the pericardium (per-i-KAR-de-um).
The pericardium holds the heart in place and helps it work properly. The sac is made of two thin layers of tissue that enclose your heart. Between the two layers is a small amount of fluid. This fluid keeps the layers from rubbing against each other and causing friction.
Pericardium
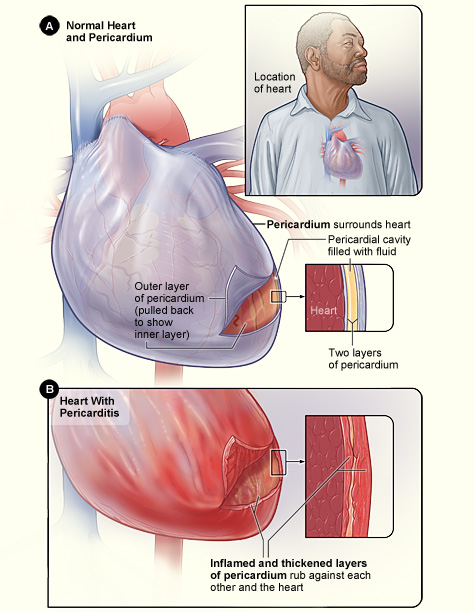
Figure A shows the location of the heart and a normal heart and pericardium (the sac surrounding the heart). The inset image is an enlarged cross-section of the pericardium that shows its two layers of tissue and the fluid between the layers. Figure B shows the heart with pericarditis. The inset image is an enlarged cross-section that shows the inflamed and thickened layers of the pericardium.
In pericarditis, the layers of tissue become inflamed and can rub against the heart. This causes chest pain, a common symptom of pericarditis.
The chest pain from pericarditis may feel like pain from a heart attack. If you have chest pain, you should call 9-1-1 right away, as you may be having a heart attack.
Overview
Many factors can cause pericarditis. Viral infections are likely a common cause of pericarditis, although the virus may never be found. Bacterial, fungal, and other infections also can cause pericarditis.
Other possible causes include heart attack or heart surgery, other medical conditions, injuries, and certain medicines. In many cases, the cause is unknown.
Pericarditis can be acute or chronic. "Acute" means that it occurs suddenly and usually doesn't last long. "Chronic" means that it develops over time and may take longer to treat.
Both acute and chronic pericarditis can disrupt your heart's normal rhythm and/or function and possibly (although rarely) lead to death. However, most cases of pericarditis are mild; they clear up on their own or with rest and simple treatment.
Other times, more intense treatments are needed to prevent complications. Treatments may include medicines and, less often, procedures or surgery.
Outlook
It may take from a few days to weeks or even months to recover from pericarditis. With proper and prompt treatment, such as rest and ongoing care, most people fully recover from pericarditis. These measures also can help reduce the chances of getting the condition again.
Other Names for Pericarditis
- Idiopathic pericarditis. This term refers to pericarditis with no known cause.
- Acute pericarditis.
- Chronic pericarditis.
- Chronic effusive pericarditis and chronic constrictive pericarditis. These are forms of chronic pericarditis.
- Recurrent pericarditis.
What Causes Pericarditis?
In many cases, the cause of pericarditis (both acute and chronic) is unknown.
Viral infections are likely a common cause of pericarditis, although the virus may never be found. Pericarditis often occurs after a respiratory infection. Bacterial, fungal, and other infections also can cause pericarditis.
Most cases of chronic, or recurring, pericarditis are thought to be the result of autoimmune disorders. Examples of such disorders include lupus, scleroderma, and rheumatoid arthritis.
With autoimmune disorders, the body's immune system makes antibodies (proteins) that mistakenly attack the body's tissues or cells.
Other possible causes of pericarditis are:
- Heart attack and heart surgery
- Kidney failure, HIV/AIDS, cancer, tuberculosis, and other health problems
- Injuries from accidents or radiation therapy
- Certain medicines, like phenytoin (an antiseizure medicine), warfarin and heparin (blood-thinning medicines), and procainamide (a medicine to treat irregular heartbeats)
Who Is At Risk for Pericarditis?
Pericarditis occurs in people of all ages. However, men aged 20 to 50 are more likely to develop it than others.
People who are treated for acute pericarditis may get it again. This may happen in 15 to 30 percent of people who have the condition. A small number of these people go on to develop chronic pericarditis.
What Are the Signs and Symptoms of Pericarditis?
Sharp, stabbing chest pain is a common symptom of acute pericarditis. The pain usually comes on quickly. It often is felt in the middle or left side of the chest. You also may feel pain in one or both shoulders.
The pain tends to ease when you sit up and lean forward. Lying down and deep breathing worsens it. For some people, the pain feels like a dull ache or pressure in their chests.
The chest pain may feel like pain from a heart attack. If you have chest pain, you should call 9-1-1 right away, as you may be having a heart attack.
Fever is another common symptom of acute pericarditis. Other symptoms are weakness, palpitations, trouble breathing, and coughing. (Palpitations are feelings that your heart is skipping a beat, fluttering, or beating too hard or too fast.)
Chronic pericarditis often causes tiredness, coughing, and shortness of breath. Chest pain often is absent in this type of pericarditis. Severe cases of chronic pericarditis can lead to swelling in the stomach and legs and hypotension (low blood pressure).
Complications of Pericarditis
Two serious complications of pericarditis are cardiac tamponade (tam-po-NAD) and chronic constrictive pericarditis.
Cardiac tamponade occurs if too much fluid collects in the pericardium (the sac around the heart). The extra fluid puts pressure on the heart. This prevents the heart from properly filling with blood. As a result, less blood leaves the heart, which causes a sharp drop in blood pressure. If left untreated, cardiac tamponade can be fatal.
Chronic constrictive pericarditis is a rare disease that develops over time. It leads to scar-like tissue forming throughout the pericardium. The sac becomes stiff and can't move properly. In time, the scarred tissue compresses the heart and prevents it from working well.
How Is Pericarditis Diagnosed?
Your doctor will diagnose pericarditis based on your medical history, a physical exam, and the results from tests.
Specialists Involved
Primary care doctors-such as a family doctor, internist, or pediatrician-often diagnose and treat pericarditis. Other types of doctors also may be involved, such as a cardiologist, pediatric cardiologist, and an infectious disease specialist.
A cardiologist treats adults who have heart problems. A pediatric cardiologist treats children who have heart problems. An infectious disease specialist treats people who have infections.
Medical History
Your doctor may ask whether you:
- Have had a recent respiratory infection or flu-like illness
- Have had a recent heart attack or injury to your chest
- Have any other medical conditions
Your doctor also may ask about your symptoms. If you have chest pain, he or she will ask you to describe how it feels, where it's located, and whether it's worse when you lie down, breathe, or cough.
Physical Exam
When the pericardium (the sac around your heart) is inflamed, the amount of fluid between its two layers of tissue increases. As part of the exam, your doctor will look for signs of excess fluid in your chest.
A common sign is the pericardial rub. This is the sound of the pericardium rubbing against the outer layer of your heart. Your doctor will place a stethoscope on your chest to listen for this sound.
Your doctor may hear other chest sounds that are signs of fluid in the pericardium (pericardial effusion) or the lungs (pleural effusion). These are more severe problems related to pericarditis.
Diagnostic Tests
Your doctor may recommend one or more tests to diagnose your condition and show how severe it is. The most common tests are:
- EKG (electrocardiogram). This simple test detects and records your heart's electrical activity. Certain EKG results suggest pericarditis.
- Chest x ray. A chest x ray creates pictures of the structures inside your chest, such as your heart, lungs, and blood vessels. The pictures can show whether you have an enlarged heart. This is a sign of excess fluid in your pericardium.
- Echocardiography. This painless test uses sound waves to create pictures of your heart. The pictures show the size and shape of your heart and how well your heart is working. This test can show whether fluid has built up in the pericardium.
- Cardiac CT (computed tomography (to-MOG-rah-fee)). This is a type of x ray that takes a clear, detailed picture of your heart and pericardium. A cardiac CT helps rule out other causes of chest pain.
- Cardiac MRI (magnetic resonance imaging). This test uses powerful magnets and radio waves to create detailed pictures of your organs and tissues. A cardiac MRI can show changes in the pericardium.
Your doctor also may recommend blood tests. These tests can help your doctor find out whether you've had a heart attack, the cause of your pericarditis, and how inflamed your pericardium is.
How Is Pericarditis Treated?
Most cases of pericarditis are mild; they clear up on their own or with rest and simple treatment. Other times, more intense treatment is needed to prevent complications. Treatment may include medicines and, less often, procedures or surgery.
The goals of treatment include:
- Reducing pain and inflammation
- Treating the underlying cause, if it's known
- Checking for complications
Specific Types of Treatment
As a first step in your treatment, your doctor may advise you to rest until you feel better and have no fever. He or she may tell you to take over-the-counter, anti-inflammatory medicines to reduce pain and inflammation. Examples of these medicines include aspirin and ibuprofen.
You may need stronger medicine if your pain is severe. If your pain continues to be severe, your doctor may prescribe a medicine called colchicine and, possibly, prednisone (a steroid medicine).
If an infection is causing your pericarditis, your doctor will prescribe an antibiotic or other medicine to treat the infection.
You may need to stay in the hospital during treatment for pericarditis so your doctor can check you for complications.
The symptoms of acute pericarditis can last from a few days to 3 weeks. Chronic pericarditis may last several months.
Other Types of Treatment
You may need treatment for complications of pericarditis. Two serious complications are cardiac tamponade and chronic constrictive pericarditis.
Cardiac tamponade is treated with a procedure called pericardiocentesis (per-ih-KAR-de-o-sen-TE-sis). A needle or tube (called a catheter) is inserted into the chest wall to remove excess fluid in the pericardium. This procedure relieves pressure on the heart.
The only cure for chronic constrictive pericarditis is surgery to remove the pericardium. This is known as a pericardiectomy (PER-i-kar-de-EK-to-me).
The treatments for these complications require hospital stays.
How Can Pericarditis Be Prevented?
You usually can't prevent acute pericarditis. You can take steps to reduce your chance of having another acute episode, having complications, or getting chronic pericarditis.
These steps include getting prompt treatment, following your treatment plan, and having ongoing medical care (as your doctor advises).
Living With Pericarditis
Many cases of pericarditis are mild and go away on their own. But other cases, if not treated, can lead to chronic pericarditis and serious problems that affect your heart. Some problems can be life threatening.
Sometimes it takes weeks or months to recover from pericarditis. Full recovery is likely with rest and ongoing care. These measures also can help reduce your risk of having the condition again.
Clinical Trials
The National Heart, Lung, and Blood Institute (NHLBI) is strongly committed to supporting research aimed at preventing and treating heart, lung, and blood diseases and conditions and sleep disorders.
NHLBI-supported research has led to many advances in medical knowledge and care. Often, these advances depend on the willingness of volunteers to take part in clinical trials.
Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions. For example, new treatments for a disease or condition (such as medicines, medical devices, surgeries, or procedures) are tested in volunteers who have the illness. Testing shows whether a treatment is safe and effective in humans before it is made available for widespread use.
By taking part in a clinical trial, you can gain access to new treatments before they're widely available. You also will have the support of a team of health care providers, who will likely monitor your health closely. Even if you don't directly benefit from the results of a clinical trial, the information gathered can help others and add to scientific knowledge.
If you volunteer for a clinical trial, the research will be explained to you in detail. You'll learn about treatments and tests you may receive, and the benefits and risks they may pose. You'll also be given a chance to ask questions about the research. This process is called informed consent.
If you agree to take part in the trial, you'll be asked to sign an informed consent form. This form is not a contract. You have the right to withdraw from a study at any time, for any reason. Also, you have the right to learn about new risks or findings that emerge during the trial.
For more information about clinical trials related to pericarditis, talk with your doctor. You also can visit the following Web sites to learn more about clinical research and to search for clinical trials:
- http://clinicalresearch.nih.gov
- www.clinicaltrials.gov
- www.nhlbi.nih.gov/studies/index.htm
- www.researchmatch.org
For more information about clinical trials for children, visit the NHLBI's Children and Clinical Studies Web page.
Key Points
- Pericarditis is a condition in which the membrane, or sac, around your heart is inflamed. This sac is called the pericardium.
- The pericardium holds the heart in place and helps it work properly. The sac is made of two thin layers of tissue that enclose your heart.
- In pericarditis, the layers of tissue become inflamed and can rub against the heart, causing chest pain. The chest pain may feel like pain from a heart attack. If you have chest pain, you should call 9-1-1 right away, as you may be having a heart attack.
- Pericarditis can be acute or chronic. "Acute" means that it occurs suddenly and usually doesn't last long. "Chronic" means that it develops over time and may take longer to treat.
- In many cases, the cause of pericarditis is unknown. Viral infections are likely a common cause of pericarditis, although the virus may never be found. Most cases of chronic, or recurring, pericarditis are thought to be the result of autoimmune disorders.
- Bacterial, fungal, and other infections also can cause pericarditis. Other possible causes include heart attack or heart surgery, other medical conditions, injuries, and certain medicines.
- Both acute and chronic pericarditis can disrupt your heart's normal rhythm and/or function and possibly (although rarely) lead to death.
- Pericarditis occurs in people of all ages. However, men aged 20 to 50 are more likely to get it than others.
- Sharp, stabbing chest pain; shoulder pain; and fever are common symptoms of acute pericarditis. Other symptoms are weakness, palpitations, trouble breathing, and coughing. Chronic pericarditis often causes tiredness, coughing, and shortness of breath. In severe cases, it can lead to swelling in the stomach and legs and hypotension (low blood pressure).
- Two serious complications of pericarditis are cardiac tamponade and chronic constrictive pericarditis. These conditions can disrupt your heart's normal rhythm and/or function. If left untreated, they may lead to death.
- Your doctor will diagnose pericarditis based on your medical history, a physical exam, and the results from tests.
- Most cases of pericarditis are mild; they clear up on their own or with rest and simple treatment. Other times, more intense treatment is needed to prevent complications. Treatment may include medicines and, less often, procedures or surgery.
- You usually can't prevent acute pericarditis. You can take steps to reduce your chance of having another acute episode, having complications, or getting chronic pericarditis. Get prompt treatment, follow your treatment plan, and get ongoing medical care (as your doctor advises).
- In some cases, it may take weeks or months to recover from pericarditis. Full recovery is likely with rest and ongoing care. These measures also can help reduce your risk of having the condition again.
- If you have pericarditis, you may benefit from a clinical trial. Clinical trials test new ways to prevent, diagnose, or treat various diseases and conditions. For more information about clinical trials for pericarditis, talk with your doctor.

